Network Marketability Matters
.png)
With Open Enrollment and AEP around the corner, one thing continues to surprise me: why aren’t health plans more focused on building marketable networks? Health plans will invest millions in expanding to new markets, dig deep to roll out the richest benefits, throw big events to court brokers—but making their networks more compelling to members is rarely the top priority.
Here’s what’s so confusing: We all know that a primary concern for buyers is the network. Do you have my doctor? My kid’s doctor? Can I go to my preferred hospital? These are the questions that drive plan selection for individuals and employers alike. In Medicare Advantage, brokers consistently cite networks as the top priority for seniors.
Yet, despite this conventional wisdom—and critical impact on revenue—health plans don’t have good answers on the strength of their network or the areas they need to improve. How many doctors do we have? How many do our competitors have? Do we have the doctors our prospective members want to see? It’s clearly important, but health plans, particularly smaller plans and new entrants, rarely know the answers.
At J2, we’ve assembled the data to answer these questions and help payers improve their network marketability. Using online provider directories and aggregated medical claims, we observe an unsurprising but overlooked relationship: network composition is a key driver of enrollment. Top enrolling plans consistently have the networks and the doctors people want. Low enrolling plans—typically smaller, regional plans—do not.
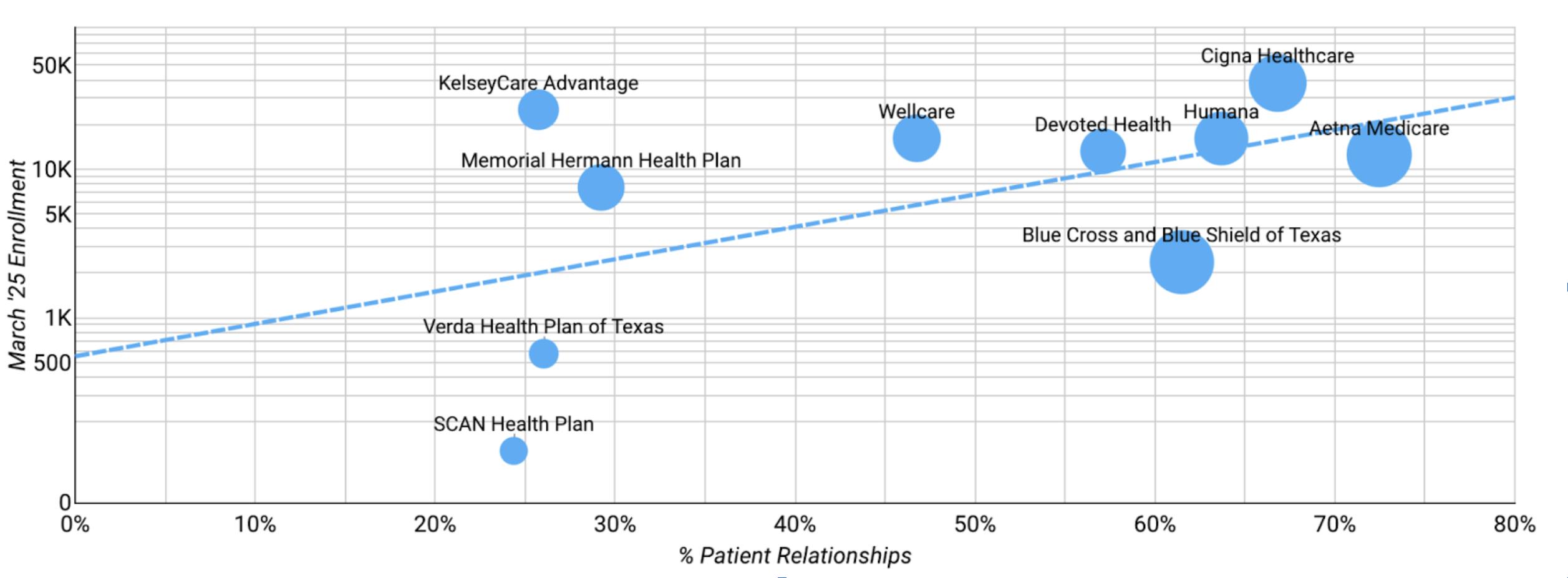
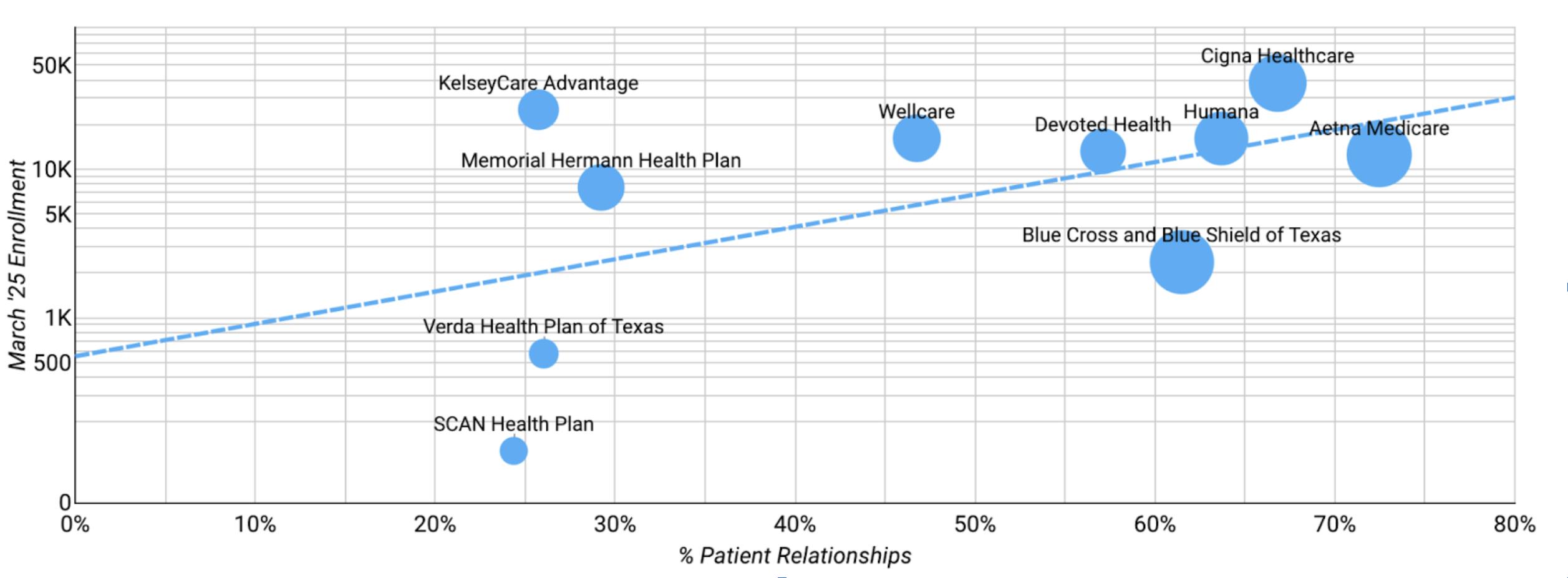
To demonstrate this, below are two charts of MA Enrollment and Network Strength for HMO plans in two of the largest counties for MA enrollment in the county - Miami-Dade County, FL (Miami) & Harris County, TX (Houston). The vertical-axes are enrollment, the horizontal-axes are network strength, measured by the # of patient relationships served by each plan’s network. The line from bottom left to top right shows the correlation between the two. The correlation is not only clear, it’s also clear that the smaller, non-national carriers are significantly disadvantaged by network.
Miami-Dade County, FL
Harris County, TX
At J2, we’ve explored the importance of provider networks on enrollment all across the country, and across all product and plan types. The relationship and importance of the network holds. Importantly, it’s not just the total number of doctors or pure network breadth that matters. What matters most is patient relationships—having a network that actually serves the target membership. You can have the richest benefits and the strongest broker relationships—but enrollment will suffer if the answer to “Do you have my doctor?” is no.
This used to be hard to fix. But today, J2 offers the data to ensure you have competitive, member-centric networks. As OE and AEP approach, it’s time to prioritize your network as a driver of growth. J2 is here to help.



